Bridging the Gap
by Kalli Dockrill | April 12, 2020
For most of us, pharmaceuticals are a product to be consumed like any other. In the rush of everyday life, we are not expected to consider how the drug was developed, how the molecules are interacting, or how the proteins are bound. We experience the physical effects with little thought as to how they came to be, or how our own physiology may impact the outcome.
But especially for those assigned female at birth, asking the right questions about the development of our medication is more important than it initially seems. The realities of human physiology mean that what we grab off pharmacy shelves won’t have the same effect on our uncles as our aunts. Sex and gender based analysis (SGBA) is an attempt to bridge this gap. Sex and gender refers to both the biological physiology of an individual (sex) and the social experiences of an individual based on their self-expression (gender). Sex-based analysis in the development of the drugs we use plays a larger role in our everyday lives than we think.
The necessity of sex-based analysis in health research became evident in 2001 with Janet Heinrich’s investigation into FDA withdrawn medications. Posicor, which was originally approved for treating angina and hypertension, significantly slowed heart rates in otherwise perfectly healthy biologically female bodies. In addition, Seldane and Hismanal, two previously approved antihistamines, were shown to cause Torsades de Points, a condition which involves prolonged intervals between contractions of the heart muscle, frequently leading to fatal cardiac arrhythmias. This side effect was more prominent in biologically female bodies: they naturally experience longer intervals between heart contractions, and lack the biologically male sex hormones which regulate the effects of this drug. A historic lack of SGBA has allowed for discrepancies in the response of different sexes to persist in widely distributed drugs. But if the detriments of this discrepancy have been clear for over a decade, why do medical researchers still neglect to conduct SGBA? Often, consumers’ lack of awareness regarding the drug development process prevents them from demanding better. It is clear that there is little guidance given to academic researchers communicating the necessity of accounting for the sex-based variability of their consumer base.
Oxford researchers remain far removed from the aisles of our local pharmacies; their research projects are often focused on such close detail that it is difficult to envision their broader impact. “An academic may have a five-year plan,” says Mark Slack, Vice President of Evotec’s Academic Partnerships, “and they’re driven by the science.” Slack emphasises that academic projects are based on academic interest and study. A researcher might concern herself with the details of protein membranes, targeting receptors far beyond the comprehension of the average drug-buying citizen. This separation may not mean much if academic research is destined only to satisfy scientific curiosity from the pages of medical journals, but that is rarely the case – least of all at Oxford, where pharmaceutical research has become increasingly commercialised.
“I really do believe that all the big breakthroughs that eventually become commercialised – eighty, ninety percent of those – are developed by unconstrained basic research that happens at universities,” says professor of chemical biology and founder of Oxford Nanopore, Hagan Bayley. Bayley says that there is clear “feedback” between fundamental and commercial research, evidenced by the rise of commercialised drug development spin-out organisations in Oxford.
Founded by Dr. Graham Richards in 1989, Oxford Molecular was one of the first spin-out organisations developed by the University, who eventually sold it in 1992. “When I set up Oxford Molecular it was a bit of a ‘naughty’ thing to do,” says Richards, but he admits that the attitude towards commercialisation has changed alongside the progression of intellectual property laws. The transfer of intellectual property rights began with the removal of the British Technology Group’s (BTG) monopolization over patents in the early 1980s. This change was first announced in 1983 where it was emphasized that although BTG no longer had first refusal on patents, an emphasis would remain on the “need for research activities to produce a commercial benefit to the UK economy”. Richards highlights that it was in 1987, when the restructuring of BTG was finally completed, that universities incurred full possession of their intellectual property. However, in Richards’ words, the condition that the research continue to provide economic benefits meant that the universities had to have “a mechanism to exploit [the research]”. Exploitation meant commercialisation. University research no longer existed for the sake of research: it became a way of entering the market. The University developed multiple spin-out organisations in which it invested shares and equity, and even though these spin-outs were made corporate, the University continued to hold seats on their committees. Among these spin-outs were such drug development companies as MirroBio, Oxford Nanopore, and Oxford Drug Development Ltd. With the commencement of commercialised research, the gap between the academic researcher and the everyday pharmaceutical consumer began to shrink.
Lab282 is currently one of Oxford’s largest accelerator schemes. Founded in November 2016, the project is a collaboration between the university, Oxford University Innovation, Oxford Sciences Innovation, and Evotec, a German based drug development company. Lab282 provides the funding needed to accelerate research into therapeutics, taking university research groups and labs and converting them into independent, corporatised spin-outs. Although Lab282 acts to provide funding to promising therapeutic research projects, the aim is not just to give “classic funding grants”: according to the VP of Academic Partnerships, Mark Slack, there is a “pure commercialization interest behind it”. “The hope and ambition is that we make new drugs out of all this…which will hopefully land one day as prescription medicine in the hospitals and beyond.” In entering the realm of Lab282 we have left behind the realm of pure academia. The gap between the academic and the consumer is effectively closed.
Which leads to the question: who is this consumer that these now-commercialised academics need to consider in their research? In December 2016 the NHS published a report on prescription drug habits in the UK. This report found that 50% of women from age forty-five to fifty-four reported taking at least one to two prescription medicines a week, in comparison with 45% of men. In the sixty-five to seventy-four age bracket, roughly 80% of women reported taking at least one to two prescribed medicines a week, and just over 50% of those women reported taking three to four prescription medicines a week.
Historically, research has not been sensitive towards sex and gender. Research focuses on cis-gendered males, and thus drug development is catered towards their physiology and experience. On the biological level, those who were assigned female sex at birth have been actively excluded. Graham Richards of Oxford Molecular admits that drugs “tend to be tested on men”. Women of childbearing age are often considered as an overly vulnerable demographic. This attitude has been adopted in legislation from as early as 1974 when the US National Research Act referred to them as “protected subjects”. Researchers worry that in a large enough sample group of women at least one or two will be pregnant, but unaware, and that any testing could potentially harm the foetus. In the name of eliminating this risk, it became industry tendency to exclude women of this demographic.
There is also the apprehension that fluctuating hormones in people with menstrual cycles will affect test results. Dr Robin Mason, who currently works furthering gender and health equity in Toronto, comments on the difficulties of integrating sex-and-gender-based-analysis into medical studies. “I think it can be complex,” says Mason. Mason notes that when you start introducing sex-and-gender-based-analysis additional variables are added, the cost of research is raised, and everything has to be run twice, which can be strenuous on time and finances. Despite these difficulties, Mason argues that SGBA is a “question of ethics in research”. “To be ethical, our research needs to consider the variability of our participants,” says Mason. “What they develop is going to be used on [people] who have reproductive cycles.”
Recent efforts, such as the 1993 NIH Revitalisation Clinical Equity Provision, have made progress towards mandating female inclusion in sample groups. However, as research moves away from human test subjects and towards animal disease systems or micrology, the sex of the broader market is forgotten. In their article on ‘Sex Bias in Neuroscience and Biomedical Research’, Annaliese K. Beery and Irving Zucker demonstrated that in 2009 the number of single-sex studies on non-human male specimens outnumbered that of female specimens at a ratio of 5.5 to 1. “In the past half-century, male bias in non-human studies has increased while declining in human studies,” writes Beery. Animal studies, however, often remain the first phase in constructing models for human studies. It is in this phase that the beginnings of analysis take place, and if this is strictly focused on biologically male specimens then the potential to understand the impact on biologically female bodies is already limited. The more small-scale the research, the less attention is given to sex-and-gender-based-differences. The Institute of Medicine reports that while “considerable attention has been given to the differences and similarities between females and males…on the level of the whole organism…scientists have paid much less attention to the direct and intentional study of these differences at the basic cellular and molecular levels.”
In 2001 Mary-Lou Pardue and Theresa M Wizemann published a guide to understanding the biology of sex and gender difference, in association with the Institute of Medicine. Pardue and Wizemann argue that sex differences go beyond the reproductive system. In a section of the report entitled ‘Every Cell Has a Sex’, Pardue and Wizemann write that differences between males and females exist on a cellular level and that these biochemical differences can largely impact health. Many of these differences are a direct result of the genetic differences between the two sexes. The report showed how symptoms and onset of cardiovascular disease are experienced differently, metabolic rates in response to toxins differ and immune and inflammatory cell responses are affected. This research continues to hold relevance. In 2016, David C. Page of Yale Medicine led research into demonstrating the extent of the genetic differences which exist on a cellular level between different sexes compounding the work of Wizemann and Pardue. Even on a molecular level sex differences must be considered and waiting until phases of testing which include human subjects to consider these differences places women at a distinct disadvantage when it comes to medical research.
The new SAGER (Sex and Gender Equity in Research) guidelines, developed by the European Association of Science Editors, attempt to address this discrepancy in sex difference. These guidelines suggest that in sex specific studies the title and abstract should specify the sex of animal cells and/or tissues used. Results should be “routinely presented and disaggregated by sex and gender” meaning that results pertaining to each sex should be presented and analysed individually in research as opposed to being generalised. The guidelines emphasise that even if no difference is noted, sex-and-gender-based analyses should still be included in reports to explain how and why this conclusion was reached. Sex differences should be considered at all levels of the research process, and any communication of the research needs to be specific and without generalisation. However, these guidelines are only as good as their implementation. They have no impact unless they are actively employed in the development of the drugs currently being produced for market, originated in accelerator schemes such as Lab282.
Lab282 has the aim of producing drugs for market. Projects can apply for up to a half a million pounds of funding towards pharmaceutical research, much of which affects the drugs that eventually make their way to consumers. This application, which requires a research proposal, contains no section referencing diversity and inclusion, meaning that there is no provision for research to contain SGBA. When asked if he was aware of the SAGER guidelines on SGBA, Mark Slack’s response made clear that he was not. When asked if the physiological difference between male and female bodies play a role in the studies being conducted, Slack answered that “if you’re looking at things like breast cancer then of course [but they’re] not classically elements that are incorporated into drug development”. These guidelines should be of increasing concern as Lab282 projects move into phases which include working with human cells and animal models. Lab282’s website boasts that Professor Shouma Bhattarcharja’s work on evasins is moving into long-term animal disease modelling. This is a case in which the SAGER guidelines would encourage researchers to begin to analyse for sex differences between the organisms and tissues they are working with, but Slack says that in this case, when it comes to specifying sex “it’s just sort of across the board”, indicating that research is applied in a generalised fashion regardless of sex and gender.
For a company which intends to eventually bring its research into public domains of consumerism, this is a worrying attitude. “We aim to be selling the research to big pharma,” says Slack, mentioning that the organisation already has contacts in place. The research is thus intended to aid thousands of individuals who take prescription medication. Yet how can research effectively do this if such a large portion of the consumer base is not being properly considered?
The aim of these spin-out drug development organisations is to bring value to the public through new and innovative medication while bringing value to the University by increasing an in-flow of profit. The University continues to hold significant minority shares in spin-out organizations. In 2017 the average initial equity stake was thirty-six percent. Profit brought into the university through these spin-outs is then funneled back to academics, various departments, and the Central University Fund. The corporatisation of these spin-outs is meant to be mutually beneficial to both the public and the university, but benefits are increasingly imbalanced when certain parties are so clearly neglected.
Research which remains in a lab is comparatively limited in its capacity to affect the population: as a result, spin-out organizations and accelerator schemes such as Lab282 can be incredibly worthwhile, boasting a high upside with a limited downside. Projects currently focused on oncology and cardiovascular medicine have the potential to help millions, and proper SGBA will only aid in this. The path to proper analysis of this kind is complicated and time-consuming. However, as opposed to viewing it as an insurmountable obstacle, sex-and-gender-based-analysis should be seen as vital to attaining the goal of these spin-outs: promoting health. In the interests of our own health we as consumers need to begin to demand that the companies developing the drugs we use look deeper into how they affect us. Our own awareness of the development of the drugs we consume is the first step in bridging the gap between the consumer and the researcher. And once we start asking questions, researchers will be reminded that we are not as far away as they think.∎
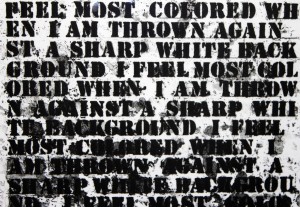
Words by Kalli Dockrill. Art by Michela Gerardin.