On Manish Shah
by Hannah Copeland | March 13, 2020
On the same day that Harvey Weinstein’s lawyers opened their defence at his heavily-covered rape trial in Manhattan, another pivotal sexual assault case drew to a close across the Atlantic: Manish Shah was sentenced to life in prison, in Court One at the Old Bailey. The jurors in both New York and London were being asked to consider complex issues around consent and power. Like Weinstein, Shah had systematically abused his position of power to prey on his victims. But unlike Weinstein, he carried out his assaults not on a casting couch, but a doctors table.
On Friday 7 February, the former GP was handed three life sentences with a minimum term of fifteen years, having been found guilty of 90 counts of sexual assault and assault by penetration against 24 female patients. The court heard how between 2009 and 2013, the 50-year-old doctor preyed on vulnerable patients’ fear of cancer to conduct unnecessary and invasive breast, vaginal and rectal examinations for his own sexual gratification. He performed the procedures without offering a chaperone, sometimes without gloves, and on one occasion leaving a patient entirely naked on the examination table. Shah, who worked at Mawney Medical Centre in Romford, east London, denied wrongdoing, claiming he had been practicing “defensive medicine”. But the prosecution detailed how Shah systematically abused his privileged access to patients’ medical records to single out victims based on their age or family history of cancer; made references to high-profile celebrity cancer cases, including to Angelina Jolie and Jade Goody, to frighten women about their health and manipulate them into consenting to invasive procedures; and falsified their medical notes to try and justify the abusive examinations. The youngest of his victims was a fifteen-year-old girl who described being left “anxious, fearful and shaking” at the prospect of visiting the doctor after being abused by Shah.
As fifteen of his victims packed into the small Court One – a historic room that has witnessed some of the most notorious defendants in British criminal history, including Ian Huntley, The Kray Twins and The Yorkshire Ripper – Judge Anne Molyneux QC addressed the gravity of Shah’s offence: “you were a master of deception and you abused your position of power. This was a horrible abuse of trust and caused incalculable harm,” she said.
With this comment, the Judge got to the heart of this case’s distinguishing feature: the longevity of the abuse – the reason victims didn’t call it out sooner – was enabled not by money or legal threats, but by trust. The courtroom in New York heard how Weinstein used nondisclosure agreements to silence his victims. The courtroom in London heard how Shah was able to perpetrate his crimes for four years because his victims were unaware that they were victims: the imbalance of power and knowledge between a patient and a doctor makes it very hard to challenge their clinical advice. In the wrong hands, trust can be weaponised.
Shah’s conviction is one of a handful of recent cases that have shone an uncomfortable light on the potential for medical professionals to abuse their patients’ trust – and for the healthcare system to fail to catch them. It comes just eight months after a high profile conviction in which a former nurse, Neils Högel, was sentenced to life for murdering 85 patients in northern Germany between 1999 and 2005; eight months after a doctor in Ohio, William Husel, was convicted of killing 25 patients by prescribing fatal doses of fentanyl; and nine months after an investigation in Ohio State University found that one of their sports teams doctors, Richard H. Strauss, had abused at least 177 men in the 1970s, 80s and 90s.
As unusual as these cases are, they raise an important question: why did no one catch the perpetrators? What needs to change to stop the next Manish Shah? The conclusion of Shah’s case coincides with the publication of a long-awaited independent inquiry report into patient safety in the British healthcare system, commissioned in the aftermath of the 2017 Ian Paterson scandal, in which the rogue surgeon had mutilated over one-thousand patients through painful and unnecessary cancer surgery. Concerningly, the report does identify major structural flaws in the British healthcare system at the root of the scandal. “It is the story of a healthcare system which proved itself dysfunctional at almost every level when it came to keeping patients safe, and where those who were the victims of Paterson’s malpractice were let down time and time again,” said Bishop Graham James, who chaired the inquiry. Specifically, the inquiry identified the disjoint between the NHS and private medical practices as one of the main reasons Paterson was allowed to “hide in plain sight”: failure to compare notes on suspicious behaviour allowed doctors to move between private and public practices, with concerns slipping through the cracks. Its chief recommendation is the creation of a single database for the entire practice of consultants, including information such as how often they have performed a particular procedure, something which the Private Healthcare Information Network and NHS Digital have confirmed they are looking into creating.
In the meantime, the impact of these few high-profile cases extends beyond their immediate consequences for the abused patients: they threaten to undermine wider public trust in the medical community. Jonathan Herring, Professor of Medical Law at the University of Oxford, expressed specific concern over the possibility of a “second class of victims to come” if patients in the future are deterred from being honest with their doctors. Dr Vivek Sharma, junior doctor, also stressed how public confidence in the medical profession is “essential for delivering effective medical care.” Britain is already grappling with falling trust in medicine as a result of targeted pseudoscience, which has recently led to an alarming fall in the take-up of routine childhood vaccines like MMR. The UK has even lost its measles-free status in recent years. It scarcely needs to be stated that a loss of trust in the medical profession has ramifications for the health and functioning of society as a whole.
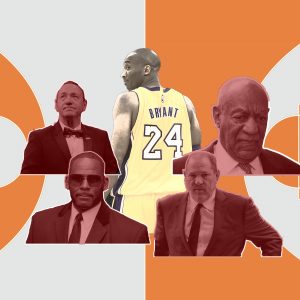
The case of Manish Shah is a historically important one. In an era in which man after man in industry after industry has been implicated in the #MeToo movement, it reveals something about the breadth of ways power can be harnessed by an abuser: not only through money, power and fame, but through trust. Manish Shah abused the trust his patients had in medical professionals to carry out his assaults. The legacy of his abuse must not be allowed to undermine wider patients’ trust in medicine.∎
Words by Hannah Copeland. Art by Deiana Hristov.